Education
Undergraduate Teaching in Orthopaedic Surgery
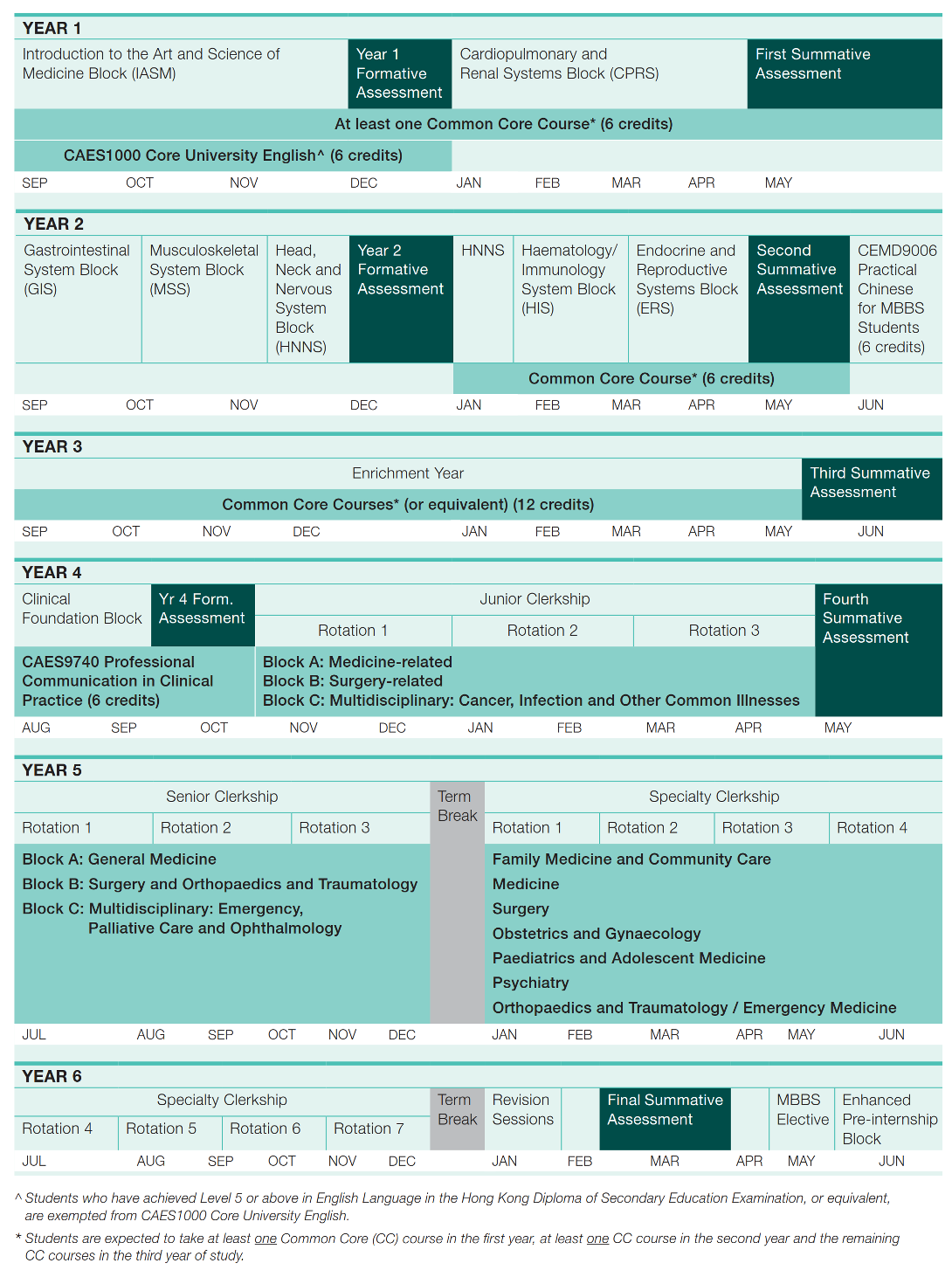
The New Medical Curriculum
The undergraduate medical curriculum was changed in 1997 and further enhanced in 2018. The most important concept and practice being introduced into the new curriculum is problem-based learning (PBL). The number of lecture is reduced, and there is increased emphasis on small group teaching. The philosophy is to cultivate life-long learning. The syllabus is therefore not comprehensive. It covers the core knowledge and skills.
Years 1 & 2
In the first 2 years of the curriculum, they go through different system blocks, one of which is the musculoskeletal system. The musculoskeletal system block is a 5 weeks module. The basic sciences are integrated with the disease processes, and the teaching sessions include PBL case tutorials, about 25 lectures (mostly basic sciences), 10 practicals (anatomy – but no need to dissect cadaver anymore; physiology; pharmacology; pathology), and a 3-hour clinical skills teaching session.
PBL case tutorial is an important element of the new curriculum. The students form small groups (usually 8 students), and go through 4 PBL cases (each case spends through 2-3 tutorial sessions). The faculty member discloses the information bit by bit. At each stage, the students discuss with one another, identify problems and learning issues. They then study and find relevant information, and return to the PBL case in the second tutorial. More information will then be provided. The faculty member may be a clinician, may be a scientist, and is usually not an expert in the field, and serves as “facilitator”. The emphasis is on “learning” (student-centered), not “teaching” (teacher-directed). The 4 cases selected are spinal muscular atrophy, humeral shaft fracture after arm wrestling, osteoarthritis of the hip, and sciatica after lifting heavy objects.
In the clinical skills session, the students are introduced to ‘look’, ‘feel’, ‘move’. They study the normal range of motions of the joints in the body on one another (Figure 1). They are also exposed to the clinical features of common conditions such as rheumatoid arthritis, osteoarthritis, gout and cervical and lumbar spondylosis.
Year 3 (Enrichment Year)
The Enrichment Year gives each student an opportunity to take charge of their learning and tailor activities to their interests and desires. Students may want to take courses offered by the Faculty and other Faculties at HKU, go on an exchange overseas, or do a research internship locally or internationally at world renowned laboratories.
Year 4 (Clinical Foundation Block and Junior Clerkship)
The Clinical Foundation Block is an 8 weeks block. The class is divided into 2 groups, one goes through 4 weeks of either medicine-related or surgery-related teaching, and then they swab. During this block, there are 4 impact lectures and 4 clinical skills sessions on orthopaedic surgery. Each clinical skills session lasts for 3 hours. The themes are 1. history taking and principles of fracture management 2. upper limbs – physical examination and common problems 3. lower limbs – physical examination and principles of joint reconstruction 4. spine – physical examination; approach to neck and back pain and recognition of major spinal problems.
The Junior Clerkship starts after Clinical Foundation Block. In junior clerkship, there are three 8-week blocks, namely medicine related, surgery related and multidisciplinary related.. Orthopaedic surgery is taught during the surgery-related block. The latter aims at better integration of certain topics, such as infection and tumour. We arrange 4 seminars, each last for 3 hours. Two of them are on tumours, and 2 are on infections of the musculoskeletal system. The format is very similar to a PBL case tutorial, except that it is a large group environment. The students are urged to learn by self-study between the two related sessions. At the same time, the students also need to attend some didactic lectures related to the musculoskeletal system.
Year 5 (Senior Clerkship)
Senior Clerkship lasts for 24 weeks and also consists of 3 blocks – General Medicine, Surgery and Orthopaedics &Traumatology and Multidisciplinary (Emergency Medicine, Palliative Care and Ophthalmology). During the Suergy and O&T block, students will attend about 15 whole class sessions on topics related to orthopaedic surgery. Nevertheless, students will be assigned to different network teaching hospitals for attachment, which include Caritas Medical Centre, Kwong Wah Hospital, Pamela Youde Nethersole Eastern Hospital, Queen Elizabeth Hospital, Tuen Mun Hospital, Princess Margaret Hospital, Yan Chai Hospital, United Christian Hospital, Tseung Kwan O Hospital and Northern District Hospital (starts in 2021). They will be divided into small groups and have 8 bedside teaching sessions. In addition, there are four interactive seminars on common orthopaedic problems, principles of fracture management, diagnostic imaging, orthopaedic emergencies etc.
Year 5 and 6 (Specialty Clerkship)
The class is divided into 7 groups and they go through 7 rotations in turn. Each rotation lasts for 7 weeks, and there are about 30 students each time. The orthopaedic surgery teaching is done together with emergency medicine. There are 17 seminars (each of 1.5 hours), 5 bedside teaching sessions, 6 out-patient new case clinics (each of 3 hours) (Figure 3), 3 clinical case conference (each of 2 hours), 1 grand rounds (each of 2 hours) and 1 OT session (each of 4 hours). In addition, students have an opportunity to work as assistant interns for 2 weeks. They will follow the daily routines (ward rounds, out-patient clinics, operations, team meeting etc.) of a house officer or a resident in one of subspecialties in O&T. For the seminars, they consist of short case scenarios; the latter are posted on the HKU Moodle and students are asked to read them and do self-learning before attending the seminar. The PBL spirit is also followed with the bedside teaching – they choose their own patients and ample time is allowed for them to revise their knowledge and skills before the teacher comes. Their skills will be assessed by a clinical competency test (Figure 2) which is conducted at the end of each rotation. It consists of 10 stations, usually 3 to 4 are X-rays / clinical photos, and 6 to 7 are on specific tests in physical examination.
Assessment and Evaluation
In the new medical curriculum, much more emphasis is put on continuous assessment of the students’ performance than before. The summative assessments are in the form of written paper and objective structured clinical assessments (OSCA). The faculty and the department are also very keen on getting feedbacks from the students. The students have so far highly rated the undergraduate teaching in orthopaedic surgery.