Services
Division of Sports and Arthroscopic Surgery
Staff
The Division of Sports and Arthroscopic Surgery is a unique division in the Department of Orthopaedics and Traumatology, The University of Hong Kong. Unlike the majority of orthopaedic surgeons who provide treatment in bone and related disorders in an open manner, sports medicine surgeons in our division are specialists in diagnosing and treating pathologies of soft tissue (e.g. tendon, ligament, capsule, cartilage, meniscus, labrum, etc) in the musculoskeletal system (e.g. hip, knee, shoulder, etc) through a minimally invasive approach with the help of an optical instrument (i.e. arthroscope).
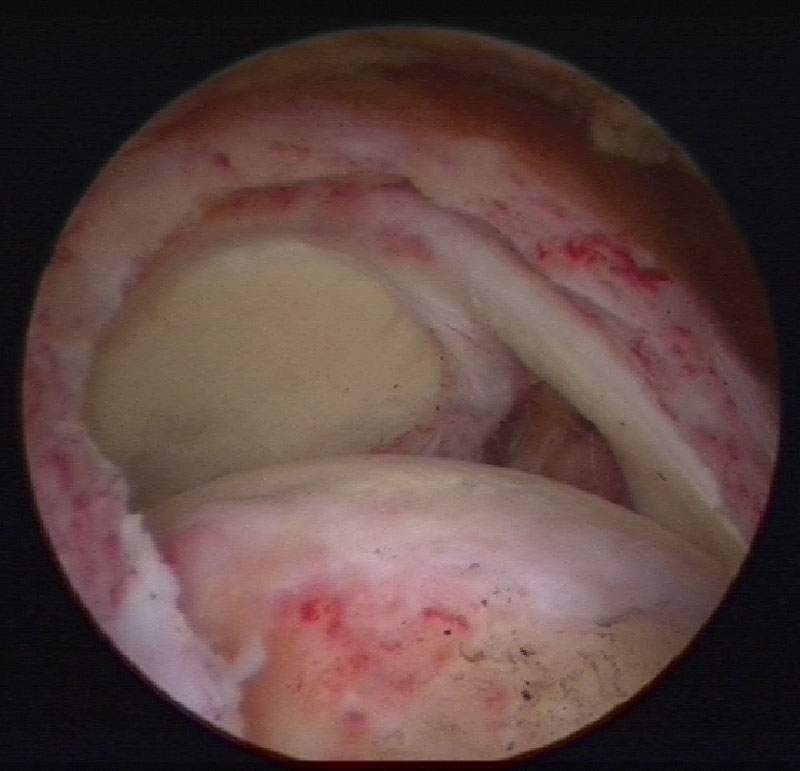
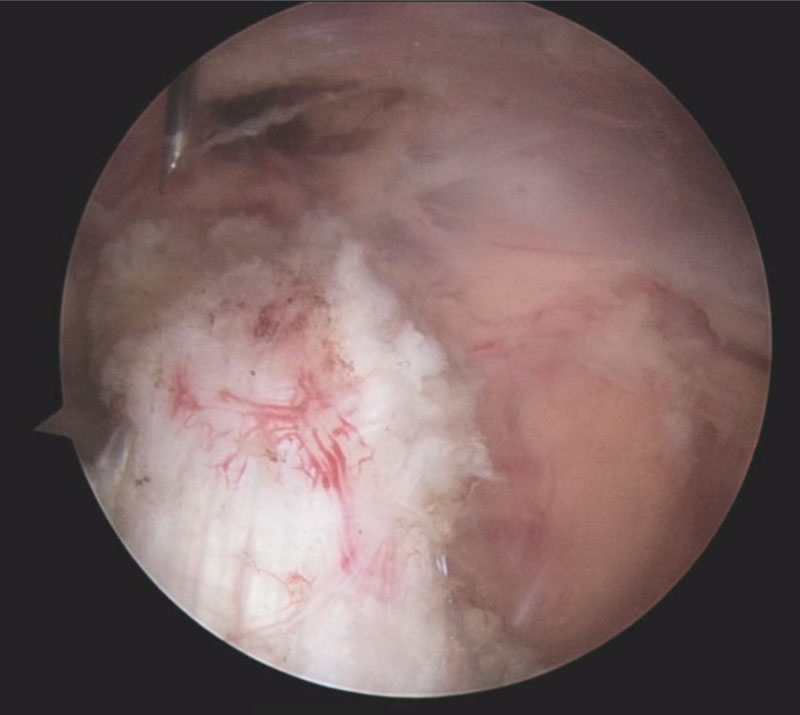
(Full thickness full width tear of supraspinatus tendon)
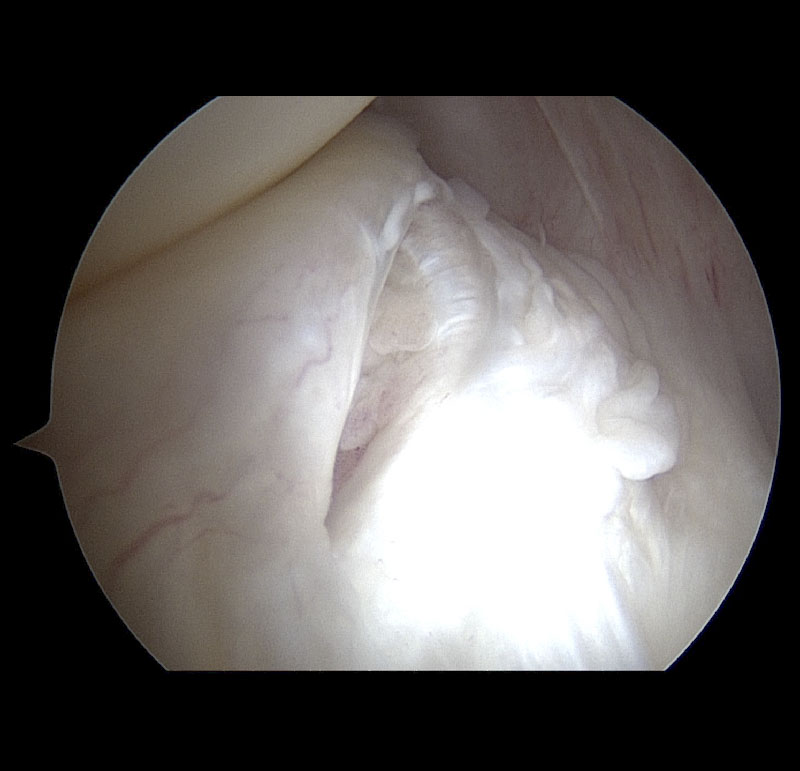
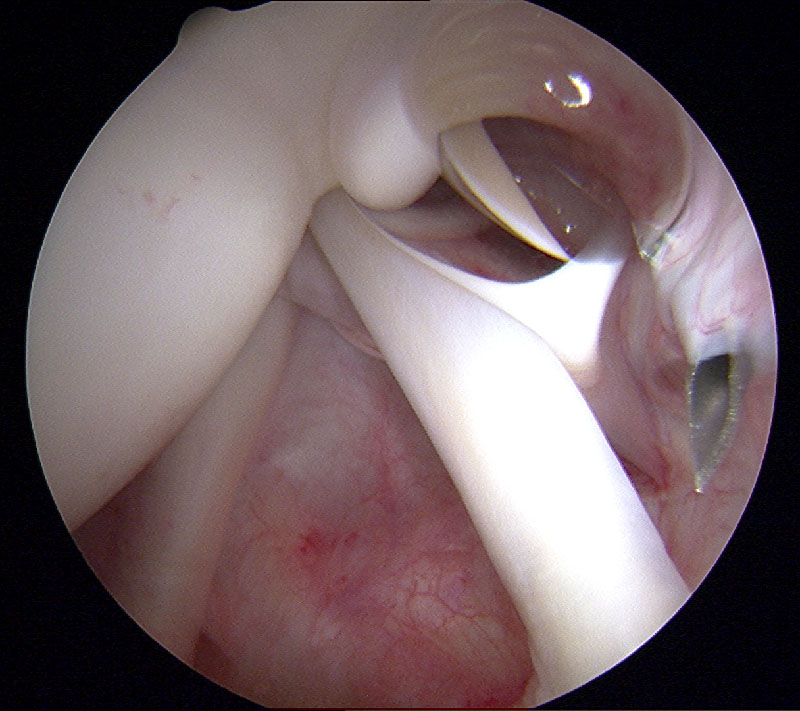
(Medial meniscus posterior horn RAMP lesion)
Overview
Arthroscopy was practiced in this department since the early 1960s. It became a much more popular technique in Hong Kong after the first “Arthroscopic Instructional Course and Workshop” held by the International Arthroscopic Association in our department in 1985.
The use of arthroscopy allows a majority of joints in human body, including the shoulder, hip, and knee, etc, to become accessible in a minimally invasive manner. Hence, it is not surprising to find that arthroscopy has become an increasingly popular method in assessment and treatment of orthopaedic problems in Hong Kong.

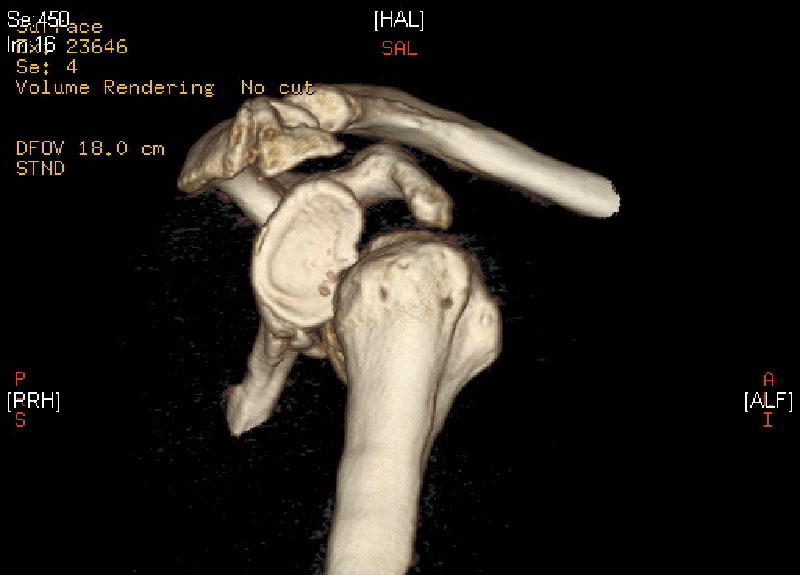
The rapid development in technology and instrumentation in arthroscopy in the past thirty years has led to the widespread application of this technique. Nowadays, the use of the “arthroscope” is no longer limited to naturally occurring body space (i.e. joint) but is extended to areas with pathologies which previously could only be assessed and managed by open surgery (e.g. endoscopic assisted quadriceps tendon repair, arthroscopic Latarjet operation, etc). The adoption of the “arthroscopic-assisted” and “endoscopic-assisted” concept in the field of orthopaedics makes the practice of minimally invasive surgery possible. The recovery of the patient is hastened and potential complications are minimized.
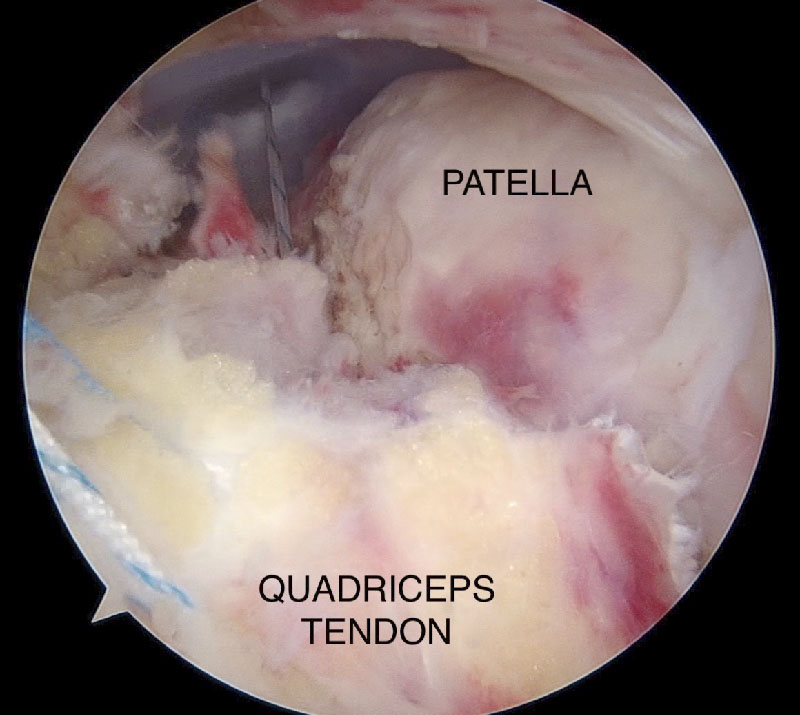
endoscopic repair of rupture quadriceps tendon
Arthroscopic Latarjet procedure
The work of the Division of Sports and Arthroscopic Surgery in the Department of Orthopaedics and Traumatology can be described using the “Three-pillars” concept, namely clinical service, teaching and research.
Clinical service
Clinical service is the most important component in the “Three-pillars”. It is because the primary duty of a doctor is to provide diagnosis and treatment to the sick and disabled. Active engagement in clinical service allows a physician to reflect on the limitations of themselves and current technology. This provides the incentive to improve, both by teaching and active participation in research.
At the current moment, Division of Sports and Arthroscopic Surgery provides service in the field of sports medicine related problem in the shoulder (including acromioclavicular joint), knee (including patello-femoral joint) and hip. The more common pathologies that we treat include: shoulder dislocation and instability, rotator cuff tear, frozen shoulder, acromioclavicular joint dislocation and arthritis, cuff tear arthropathy of shoulder, isolated cartilage injury of knee, meniscal tear, quadriceps tendon rupture, patellar tendon rupture, anterior cruciate ligament tear, posterior cruciate ligament tear, patellar dislocation and instability, hip labral tear, snapping hip, etc.
We conduct six outpatient clinics for the general public every week, including one general outpatient clinic, two sports outpatient clinics (one on shoulder, one on hip and knee), one pre-operation assessment clinic, one post-operation clinic and one new case clinic. We provide care to a total of more than 2,000 outpatients each year.

The Division runs four operation sessions each week. We operate a total of 150 to 200 surgeries each year. These include arthroscopic assisted shoulder surgery (including Bankart repair, SLAP repair, Latarjet procedure, rotator cuff operations, biceps tendon surgery, repair and reconstruction of acromioclavicular joint dislocation, etc), open shoulder surgery (e.g. reverse total shoulder arthroplasty), arthroscopic assisted knee surgery (including meniscal operation, cartilage operation, anterior cruciate ligament reconstruction, etc), endoscopic assisted knee surgery (including repair of extensor mechanism rupture, repair of medial patello-femoral ligament tear, etc) and open knee surgery (including high tibial osteotomy, Fulkerson osteotomy, trochleoplasty, etc). A majority of the surgeries (over 95%) are done in a minimally invasive manner with the help of an arthroscope. The length of in-patient hospitalization is typically short. Day surgery is practiced in selected cases.


Teaching
We believe that it is important to teach our next generations the correct approach and essential knowledge in managing patients with sports medicine problems. Over the years the division has been heavily involved in the teaching of medical students, post-graduate students, orthopaedic trainees, as well as local and overseas orthopaedic fellows.
The division is responsible for providing regular teaching to local medical students and overseas exchange students in the area of shoulder and knee problems throughout the curriculum. The total teaching contact hours are around 1,000 student-hours per year.

The division is also involved in teaching trainees working at Hospital Authority (including those in basic surgical training program and higher orthopaedic training program). With the collaboration of the Hong Kong College of Orthopaedic Surgeons, teaching conferences, sports medicine related clinical tutorials and theme-based educational days are conducted regularly by our division. A total of more than 250 trainees were taught by us in the past ten years.
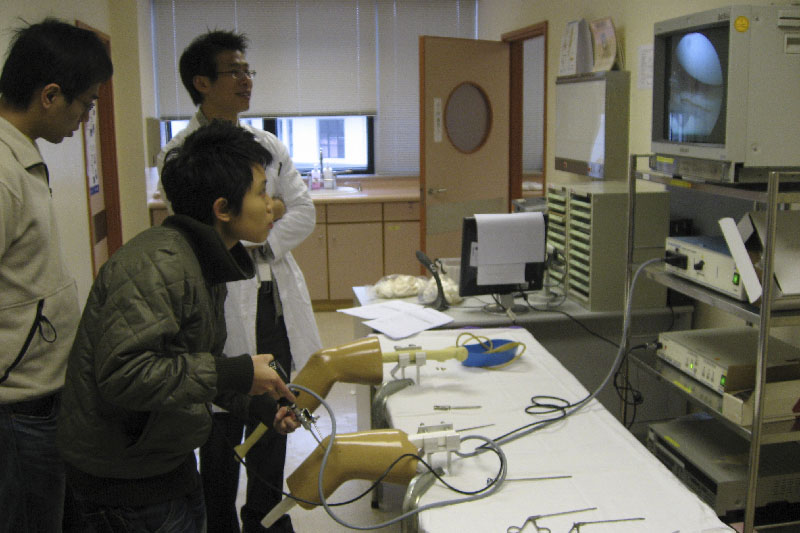
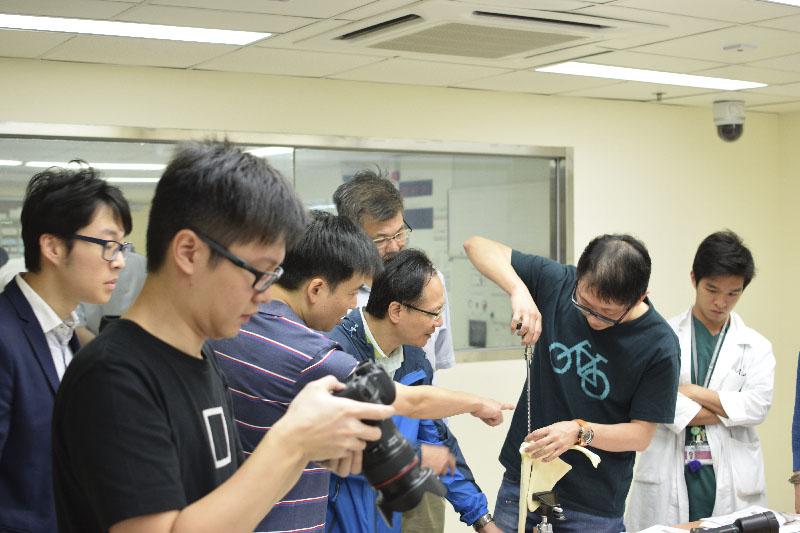


The division provides skill-based teaching to orthopaedic surgeons (both local and overseas) by organizing and teaching cadaveric workshops concerning the arthroscopic surgery of the knee and shoulder. We have been involved in running more than 10 cadaveric workshops in the last decade. Over 150 orthopaedic surgeons were trained.


Research
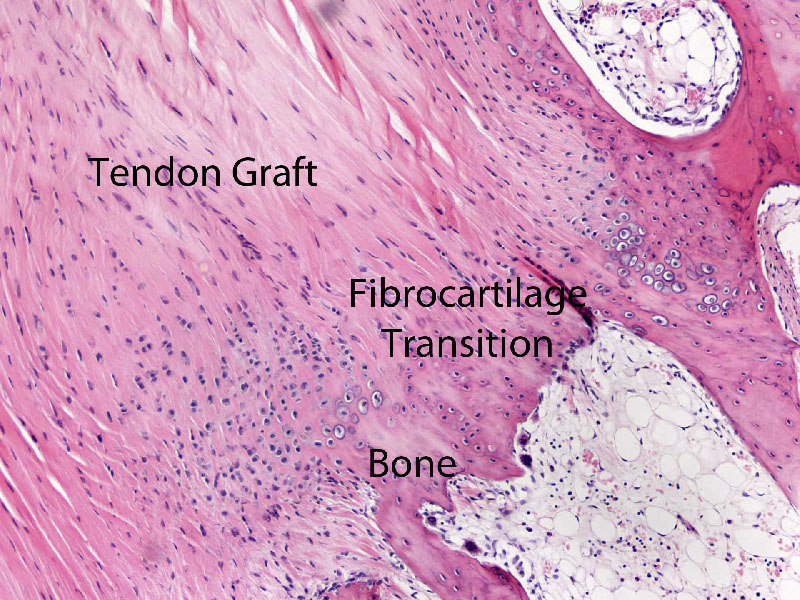
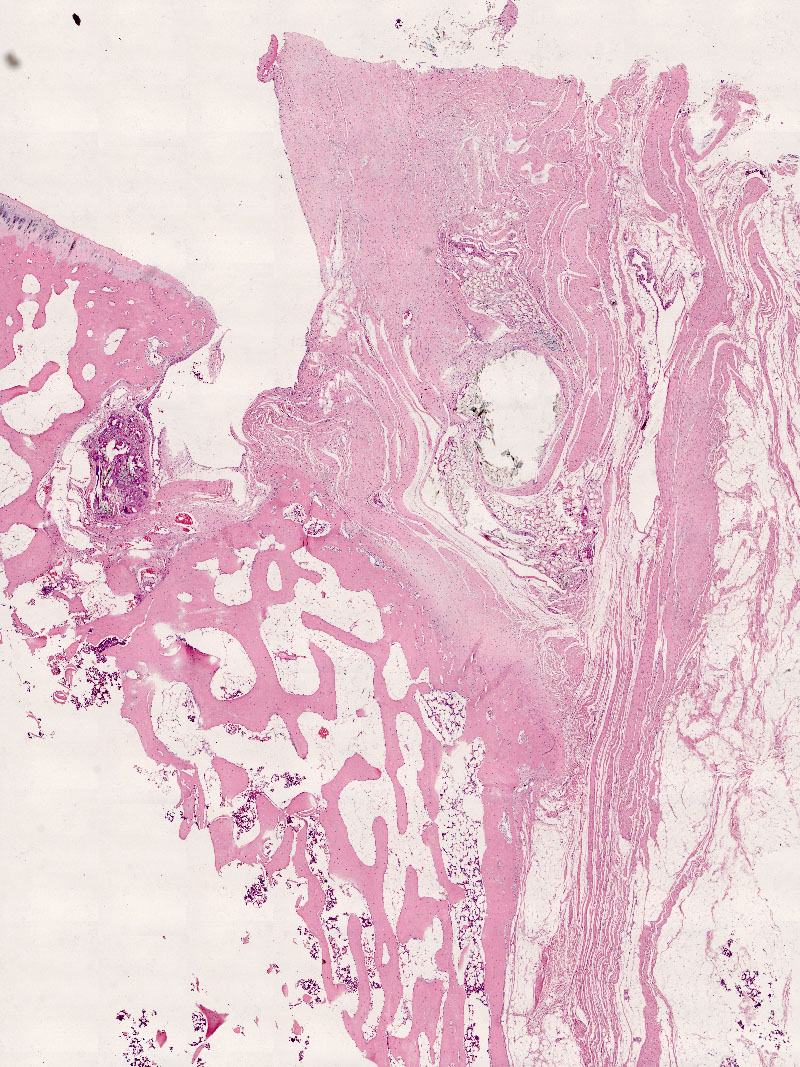
Despite the fact that anterior cruciate ligament reconstruction is a commonly performed operation, significant issues in terms of suboptimal graft incorporation within the bone tunnel, lack of suitable tools for outcome assessment and potential inaccuracy in tunnel position are still areas that receive a lot of attention. Many surgeons believe that there is still much room for improvement in this most commonly performed operation in the field of Sports Medicine. In order to address this, Division of Sports and Arthroscopic Surgery is now investigating possible methods in improving the result of ACL reconstruction, through both the basic science approach (e.g. enhancing graft incorporation in ACL reconstruction using strontium and stem cell technology, improving precision of tunnel position placement through computer navigation surgery) and the clinical approach (by developing new surgical method in ACL reconstruction). The classic “pivot shift” test is now revisited using motion analysis technique. We believe that this will lead to a better understanding in ACL reconstruction surgery and will hopefully result in improvement in the standard of care in this commonly performed operation.

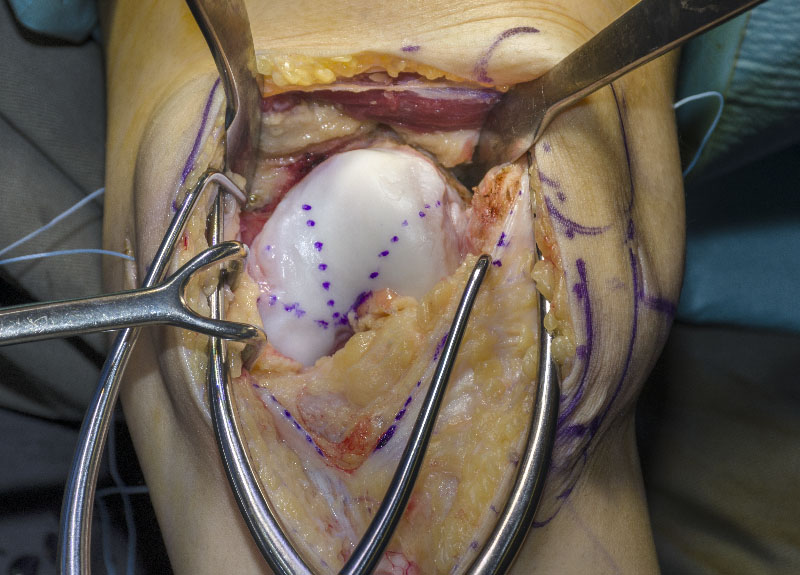
Management of chondral lesion is currently a popular topic of discussion in the world of orthopaedics. Autologous chondrocyte implantation is considered to be the standard of care. Despite of the high cost, the regenerated tissue is still far from optimal. We are now working with the Department of Medical Engineering of the University of Hong Kong to explore the possibility of combining a novel scaffold and stem cell technology in treating this issue. We hope that this will result in an ultimate solution for this difficult clinical problem.
Rotator cuff tear can be found in over half of the population at or older than sixty-years old. The result of surgical repair is suboptimal with a reported failed healing rate ranging from 20% – 70%. The relatively slow healing of diseased tendon in the tendon-bone interface and the suboptimal mechanical property of degenerated tendon are considered to be the two main reasons of this high failure rate. We are investigating along the lines of improving the result of rotator cuff repair by stimulating tendon-bone healing by biological augmentation, strengthening tendon-suture interface by developing new methods of repair as well as new methods of tying arthroscopic knots. The researches are conducted in both the areas of basic science and clinical study.

Basic Science Research
- Role of Strontium in interfacial tissue engineering in tendon healing and ligament reconstruction
- Biomechanical study of a new arthroscopic knot – “HK-knot”
- Feature based 2D-3D registration and 3D reconstruction via statistical inference for image-guided interventions
Clinical Research
- Development of new surgical technique for knee and shoulder surgery
- Combined Anterior cruciate ligament reconstruction and anterior-lateral ligament reconstruction
- Osteometry of Chinese and its impact in orthopaedic disease and intervention
- Computer navigation orthopaedic surgery